Engaging with patients at all levels
Nov. 2019Engaging with patients
Gesetzesgrundlage. Patient engagement is an important challenge, and one that the FOPH is keen to support. There are various ways of engaging with patients and their relatives, ranging from the micro level, where professionals and patients hold one-to-one discussions, through to the macro level, where patients and their families may be asked to provide input for new draft legislation, for example.
Patient engagement – i.e. involving patients and their families in healthcare provision – is becoming increasingly important at global level. Engagement has been called the “Holy Grail of healthcare provision” or the “blockbuster drug of the decade”. While these claims are doubtless exaggerated, professionals all agree that involving patients and their families is important. Without greater patient engagement, it will be difficult to streamline our healthcare system and gear it more effectively to people’s needs.
Patient engagement is a subject that is constantly cropping up at the FOPH. One of the things that set the ball rolling was the Federal Council’s Health2020 strategy, which explicitly places people at its centre, stating that “The health system needs to continue to develop around them and their needs”. Engaging with health insurance policyholders and patients is essential in delivering a successful outcome to health policy reforms.
There are various reasons for stepping up engagement with patients and their families. One is that engagement increases the efficacy of treatment and improves care, as the Chronic Care Model demonstrates. Developed in the 1990s, the model provides an efficient way of delivering high-quality care to chronically ill patients. It comprises five elements, one of which is self-management support for patients. The aim is not to tell them what they have to do, but to help them take responsibility for their own health. It is important for patients to be informed of their illness so that they can make decisions autonomously. Furthermore, selfmanagement has been shown to be cost-efficient when combined with care from the patient’s GP.
The question now is how to increase patient engagement in our healthcare system? How can professionals work more “with” rather than “for” patients? The Montreal model, developed at the University of Montreal’s Faculty of Medicine, delivers answers to these questions.
Levels of patient engagement
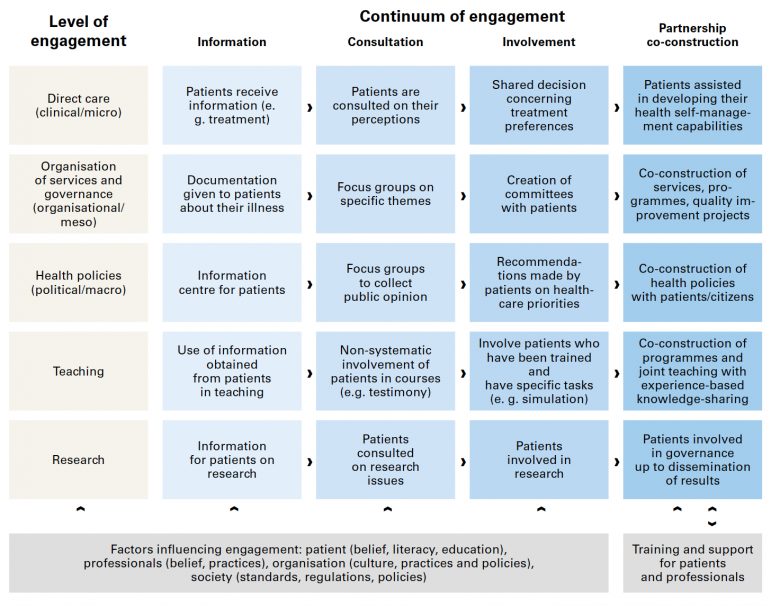
The first level of engagement is information – when a professional informs a patient about the treatment, for example. There is little dialogue at this level, which is a paternalistic form of engagement. The next level is consultation, where the professional solicits the patient’s views and the patient has an opportunity to ask questions. At this level of engagement, patients assume a more active role by participating in decisions. At the partnership level, patients are aided in recognising their own capacities and using them for the benefit of their health.
The idea now is not to automatically turn every engagement into a partnership. A partnership-based approach does not make sense in all cases, all levels of involvement will continue to be legitimate in the future. However, a growing number of patients will want partnership-based involvement. This may also impact future treatment. For example, a study of patients with cardiac arrhythmia revealed that the patients who were involved in decision-making opted for fewer invasive procedures.
The introduction of electronic patient records (EPRs) in Switzerland may also affect engagement, in addition to exemplifying the shift towards a more active role for patients. In the past, the professionals held all the data and patients were granted access to it. EPRs will change that. Instead, patients will have control of their own records and will grant professionals access to them.
Organisational levels
The diagram not only shows the continuum of patient engagement, but also the levels at which it can occur. These start with the micro level, at which there is face-to-face dialogue between patients and professionals. The next level encompasses healthcare facilities such as hospitals and care homes. Here patients can contribute to improving everyday hospital processes or the quality of communications, updating care home recommendations or providing input for the training given to healthcare professionals. To make this a reality, a growing number of Swiss hospitals are setting up Patient Advisory Boards. Efforts to involve patients and their families in the planning, implementation and evaluation of health promotion projects can be seeded at this level. The macro level aim is to engage patients at communal, cantonal and national level in improving health laws or helping determine how resources are allocated.
Engaging with patients and their families at the FOPH
While the FOPH does not systematically engage with patients and their families, this edition of spectra does show that a number of initiatives are underway. Proposals for the “Prevention in healthcare provision PHP” project will be scrutinised to ensure that the projects chosen for funding provide for patient engagement. Furthermore, self-management has been designated within the PHP projects as an area requiring priority action (priority intervention area). In addition, the FOPH also works directly with people who are personally affected and/or their families on other projects – such as female genital mutilation or suicide prevention – or ensures during the award process that projects include engagement.